 Ankle Injuries
Ankle Injuries
The ankle is the most injured peripheral joint in the body. Ankle injury ranges from 15% to as high as 59% of all injuries in some sports. The sports that most commonly produce high ankle injury rates in their participating athletes include: basketball, netball, and the various codes of football. Thus those sports and other activities that involve running, balance and quick stop-start movements appear to be of higher risk. There is a two-fold increased chance of ankle injury in those that have previously sustained an ankle injury compared to those that have not.
Injury
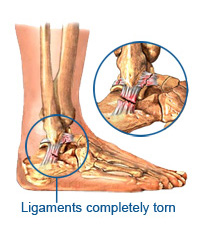
The mechanisms of ankle ligament injury are varied but are commonly due to inversion coupled with plantar flexion. Thus, lateral ankle ligament injury is most common and is often associated with peroneal tendon strain or rupture. Lateral ankle ligament injury account for in excess of 40% of all ankle injuries. Medial ankle ligament injuries are less common. This is due to the strength of the deltoid ligament and structure of the ankle joint itself. However, medial injury may occur with excessive pronation, eversion and dorsiflexion, or pronation and external rotation. These movements may also induce sprains to the ankle syndesmosis, such injury only occurs in 10% of ankle injuries. If there is a history of compressive forces to the mortise, osteochondral damage needs to be ruled out. Ligament injury is graded depending on the degree of damage. Grade 1 injuries cause stretching of the ligament without macroscopic tear, and the joint is considered stable on testing. Grade 2 injuries consist of partial macroscopic tearing with mild to moderate instability. Moderate swelling and tenderness are present and the functional ability is compromised. The Grade 3 sprain involves complete ligament rupture associated with marked swelling, ecchymosis and instability. Differential diagnosis of lateral ankle injury: Pain that persists following an acute lateral ankle sprain should alert the clinician to the possibility of other injury concomitant with the ligament injury. The differential list should include several possibilities not limited to: chronic instability, early degenerative joint disease, loose bodies, osteochondral lesions, occult fractures, intra-articular meniscoid lesions and peroneal tendon injury (including tendinitis, rupture and subluxation).
Assessment
A detailed history is needed to determine mechanism of injury. The patient may often describe a ‘crack’ or popping sound. This, along with the level of swelling is a good indictor of severity. Often with a sprain, the patient is able to weight-bear immediately after the injury, and often report continuing activity. Site of pain gives a good indication of the tissues damaged. Special tests such as anterior draw (moving talus anterior), talar tilt (moving the talus laterally and medially) and proprioception are used to assess the degree of ankle integrity. The Ottawa ankle rules on X-Ray imaging are used to determine if an X-Ray is required.
Treatment Types
Treatment regimes for lateral ankle sprain are indeed quite varied. The injury type often dictates the form of the treatment, but in many cases, several approaches have been used for the same injury. The most commonly used forms of treatments are mobilisation, immobilisation, and surgery. Mobilisation:
Rehabilitation
The program goals are to minimize the effusion, normalize gait, normalize pain-free range of motion, prevent muscular atrophy, maintain proprioception, and maintain cardiovascular fitness. Most methods involve a 3-phase treatment regime started as soon as the injured ankle is seen. Phase One
For further information on Ankle Injuries and Professional Treatment available at Synergy Healthcare contact us today. CONTACT US